Could our poor eating habits be contributing to feelings of anxiety or depression? A burgeoning body of research focusing on the connection between the gut and the brain suggests that something as prevalent as anxiety might find relief through the consumption of foods that foster a healthier balance of gut bacteria.
In recent scientific explorations, a burgeoning body of research has unveiled compelling links between specific microbiota – the diverse ecosystem of microorganisms within our bodies – and a gamut of health conditions. These connections traverse the realms of mental health, reaching as far as influencing depression and even impacting inflammatory responses within our physiology. The revelation of these associations underscores the paramount importance of embracing a diet rich in a wide spectrum of nutritious foods, crucial for fostering the complete array of microbiota necessary for our optimal functioning and flourishing.
The intricate dance between gut health and mental well-being beckons us to delve deeper into understanding their symbiotic relationship. How, precisely, do these intricate systems collaborate to wield such a profound influence on our holistic health?
The gut, often hailed as the “second brain,” plays a pivotal role beyond mere digestion; it harbors a diverse community of microorganisms that actively communicate with our central nervous system. This communication network, known as the gut-brain axis, serves as a bidirectional highway where signals and biochemical messages flow between the gut and the brain.
The ramifications of this dynamic interaction are far-reaching. Research increasingly suggests that the state of our gut health profoundly impacts our mental and emotional well-being. Imbalances or disruptions in the gut microbiota composition have been associated with an increased susceptibility to mental health disorders, including depression, anxiety, and even conditions like stress.
The intricate interplay between gut health and mental health doesn’t operate in isolation. Rather, it extends its influence across various physiological pathways. For instance, certain strains of gut bacteria produce neurotransmitters, including serotonin, often referred to as the “happy hormone,” influencing mood regulation. Additionally, the gut microbiota actively participates in the synthesis of vital compounds, such as short-chain fatty acids, with known anti-inflammatory properties that contribute to overall health and well-being.
Understanding the symbiosis between these systems underscores the significance of a well-rounded diet. An emphasis on diverse, nutrient-dense foods supports the proliferation of a robust and diverse gut microbiome, promoting a healthy gut-brain axis. This dietary approach, laden with prebiotics and probiotics from a variety of sources, serves as a cornerstone in fostering an environment conducive to optimal mental and physical health.
Furthermore, the recognition of this intricate relationship opens avenues for novel therapeutic interventions. Strategies focusing on modulating gut health, such as dietary modifications, targeted probiotic supplements, and emerging fields like gut microbiota transplantation, hold promise in the realm of mental health management and overall wellness.
In essence, the profound link between gut health and mental well-being offers a compelling narrative, urging us to recognize and embrace the intricate connections within our bodies. Nurturing our gut through mindful dietary choices emerges not just as a pathway to physical vitality but as a pivotal component in nurturing our mental resilience and emotional equilibrium.
Gut Health And Anxiety
Researchers at the Shanghai Medical Health Center undertook an extensive review encompassing more than 21 studies to delve into the impact of food, spanning both probiotic and non-probiotic aspects, on the realm of anxiety. The comprehensive analysis scrutinized various approaches and their efficacy in mitigating anxiety levels.
Among the array of studies scrutinized, a notable observation emerged: of the 14 studies integrating probiotics, a mere 36% yielded positive outcomes in terms of anxiety reduction. Conversely, a fascinating trend surfaced within the realm of non-probiotic methods, particularly those revolving around dietary adjustments. Of the seven studies exploring dietary modifications, six revealed significant effectiveness in curbing anxiety levels. This revelation sparked intriguing contemplation among the researchers, leading them to speculate on the potential superiority of altering dietary habits to diversify energy sources. Such a dietary shift might ostensibly foster the growth of a healthier spectrum of gut bacteria, surpassing the effects of singularly administered probiotic supplements with specific bacterial strains.
Moreover, the researchers advocate for a broader approach to anxiety treatment, proposing the regulation of intestinal flora as an adjunctive strategy alongside conventional psychiatric medication. Their recommendation encourages a holistic view, suggesting that balancing intestinal microbiota could serve as a supplementary avenue for alleviating anxiety symptoms.
Echoing this sentiment, insights from Time Magazine underscore the pivotal role of dietary choices in nurturing a fulfilling and enduring life. Embracing a Mediterranean-style diet, characterized by a harmonious blend of lean proteins, fruits, vegetables, pulses, and Omega-3 fats, emerges as a cornerstone for fostering not just a hospitable environment for beneficial microbiota but also for maintaining optimal cardiovascular health. The importance of maintaining a healthy weight cannot be overstated, particularly in the face of escalating obesity rates. Thus, prioritizing the nurturing of gut health through a diverse, nutritious diet emerges as a prudent and holistic decision, extending its benefits across all age groups, from children to adults. This underscores the transformative potential of dietary adjustments as a multifaceted approach toward well-being, encompassing mental and physical health alike.
Gut Bacteria And Depression
In the February 2019 issue of Nature Microbiology, a research study, highlighted in VIB, delved into the intricate connection between specific gut bacteria and the prevalence of depression. The findings illuminated a consistent pattern among individuals grappling with depression, showcasing diminished levels of two specific microbiota: coprococcus and dialister. This correlation between gut bacteria composition and mental health suggests a potential link between these microbiota and the onset or progression of depression.
The significance of maintaining a diverse array of gut bacteria emerged as a crucial factor with potential protective effects on brain health. Mireia Valles-Colomer, in emphasizing the multifaceted impact of various microorganisms, highlighted their distinct and potentially beneficial effects on different bodily systems. Notably, certain substances produced by these microorganisms, such as by-products of ‘feel-good’ neurotransmitters like dopamine, have been associated with fostering a higher quality of mental well-being.
This revelation underscores the intricate interplay between gut microbiota and mental health, shedding light on the potential mechanisms by which specific bacteria, or their by-products, could influence mood regulation and overall mental quality of life. The emerging understanding of these connections suggests a nuanced approach to mental health management, potentially involving interventions that target and modulate gut microbiota to positively impact mental well-being.
Depleted Microbiota Levels Disrupt Brain Connection
Before 2019, the scientific community acknowledged the undeniable correlation between gut well-being and mental health without comprehensively understanding the underlying mechanisms. However, a groundbreaking study conducted by researchers at Weill Cornell Medicine and Cornell’s Ithaca Campus in 2019 provided profound insights into this enigmatic relationship. This revelation stemmed from an exploration into the intricate molecular connections bridging the gut and the brain.
The study’s focal point involved administering antibiotics to mice, effectively reducing their levels of microbiota. Astonishingly, these microbiota-depleted mice exhibited a significant impairment in their ability to learn the cessation of danger signals, unveiling a crucial facet of the gut-brain nexus. Researchers discerned that diminished microbiota levels triggered genetic alterations within cells, disrupting the intercellular communication crucial for the formation of neural connections—a fundamental process underpinning learning mechanisms.
Beyond merely uncovering the impact on learning, the study unearthed a more intricate landscape. Specific substances associated with neurological disorders such as schizophrenia and autism displayed discernible changes in mice harboring depleted gut bacteria. This revelation hinted at the profound influence gut microbiota could wield over the biochemical milieu implicated in various mental health conditions.
The profound implications of this study extend far beyond a mere association between gut microbiota and mental health. It underscores a pivotal link between microbiota levels and the intricate web of cellular activities that govern cognitive processes. This newfound understanding illuminates the potential role of gut health in modulating neural connections and biochemical pathways, thereby shaping mental well-being and laying the groundwork for potential interventions targeting gut microbiota to mitigate the risk or progression of mental health disorders.
What Foods Promote Good Gut Health?
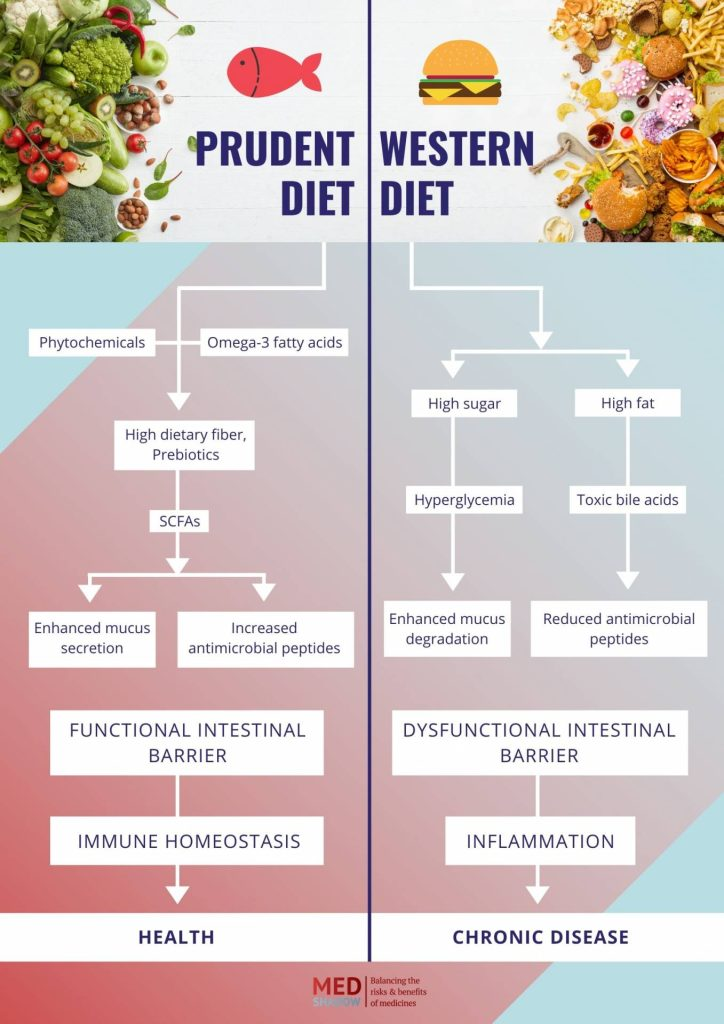
The Mediterranean diet has emerged as a versatile and enriching approach to diversify the spectrum of foods introduced to the gut. Central to this dietary regimen is the pivotal role of fiber, a crucial component that holds immense significance in fostering gut health. Research delineated in the Cell Host & Microbe Review underscores a stark contrast between the Mediterranean diet and the prevalent Western dietary patterns. While the Western diet tends to be deficient in fiber yet abundant in elements like sugar, fat, emulsifiers, and red meat, it inadvertently fosters an environment conducive to the production of detrimental byproducts detrimental to microbiota growth.
Conversely, diets emblematic of the Mediterranean paradigm, characterized by the inclusion of fish in lieu of red meat, seasonal fruits and vegetables, probiotics, and healthy fats, lay the groundwork for optimal microbial conditions within the gut. These dietary choices facilitate the proliferation of vital peptides and fortify the immune response, nurturing a harmonious environment for beneficial microbial activity.
The repercussions of dietary habits extend far beyond mere gut health. High-sugar, processed food diets serve as catalysts for inflammation—a pervasive factor implicated in an array of health issues ranging from premature skin aging to cardiovascular diseases. Scientists highlight that prolonged deprivation of dietary fiber disrupts the integrity of the mucus barrier, creating a breeding ground for bacteria that exacerbate its degradation. Compromised mucus barriers render us more vulnerable to infections by compromising our body’s natural defense mechanisms.
Therefore, the adoption of a high-fiber, low-sugar dietary regimen assumes paramount importance, transcending its role not only as a catalyst for enhancing mental health but also as a formidable fortification for the immune system. Such dietary choices serve as a formidable shield against the onset of numerous ailments, including obesity, diabetes, and even respiratory conditions like lung disease and asthma. Embracing this dietary ethos emerges as a holistic approach, nurturing overall well-being by fortifying both mental and physical health.
Conclusion
Recent research has traversed significant milestones in unraveling the intricate correlation between gut health and the expansive realm of mental well-being. Among the myriad mental conditions prevalent globally, anxiety and depression stand out as prime examples intertwined with gut health. Moreover, the implications of gut health extend beyond mental landscapes, encompassing an array of chronic diseases capable of diminishing both longevity and quality of life.
To fortify both mental acuity and physical vitality, prioritizing a nourishing and diverse dietary intake emerges as a pivotal strategy. Incorporating a spectrum of nutrient-rich foods while integrating probiotic elements into daily or weekly dietary regimens offers a promising avenue toward bolstering overall health. This strategic dietary approach not only nurtures a thriving gut environment but also holds the potential to positively influence mental health and resilience against various chronic ailments.
Embracing a dietary paradigm rich in diversity and augmented by probiotic components stands as a proactive measure toward fostering a harmonious interplay between gut health and mental well-being. This proactive approach not only serves as a cornerstone for optimal health but also represents a proactive step toward preserving mental acumen and fortifying resilience against chronic health challenges.










